Fulminant rhinocerebral mucormycosis in a patient with metabolic comorbidities: an unusual case report
DOI:
https://doi.org/10.24265/horizmed.2025.v25n3.12Keywords:
Mucormycosis , Lung Diseases, Fungal , Invasive Fungal Infections , Diabetes MellitusAbstract
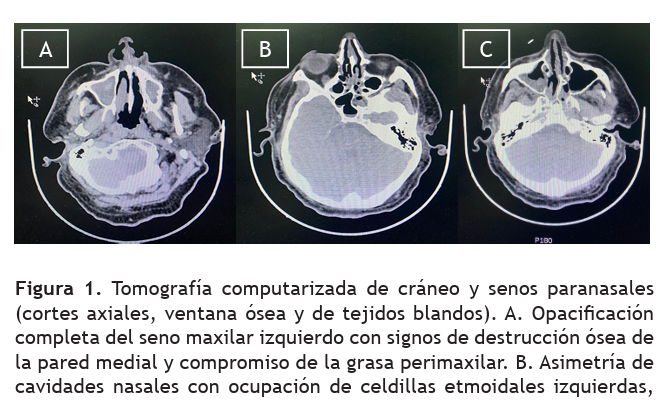
Mucormycosis is a rare but fulminant invasive fungal infection caused by fungi of the order Mucorales. It primarily affects patients with risk factors such as diabetes mellitus, hematologic malignancies, solid organ or hematopoietic stem cell transplantation, and prolonged immunosuppressive therapy. Its various clinical forms include the rhino-cerebral presentation, one of the most aggressive, characterized by rapid local progression with involvement of orbital, neurological and vascular structures, and high lethality if not diagnosed and treated promptly. We present the case of a 53-year-old male patient with a history of poorly controlled type 2 diabetes mellitus, who sought medical attention due to severe headache, right periorbital edema, and diplopia that had been present for 72 hours. A computed tomography (CT) scan of the paranasal sinuses revealed occupation of the left sphenoid sinus, adjacent soft tissue thickening, and signs of bone erosion of the lamina papyracea. These findings prompted nasal endoscopy with tissue sampling for histopathological analysis, which confirmed the presence of broad, non-septate hyphae with right-angle branching, consistent with rhinocerebral mucormycosis. Systemic antifungal therapy with liposomal amphotericin B was initiated, and endoscopic surgical debridement of the affected tissues was performed. Despite a multidisciplinary approach and timely implementation of therapeutic measures, the patient experienced rapid neurological deterioration, with impaired consciousness, and died a few days after admission. This case underscores the need for high index of clinical suspicion in patients with complicated rhinosinusitis and predisposing factors, as well as the urgency of diagnosis and treatment to improve prognosis.
Downloads
References
Cornely OA, Alastruey-Izquierdo A, Arenz D, Chen SCA, Dannaoui E, Hochhegger B, et al. Global guideline for the diagnosis and management of mucormycosis: an initiative of the European Confederation of Medical Mycology in cooperation with the Mycoses Study Group Education and Research Consortium. Lancet Infect Dis. 2019;19(12):e405–e421. Disponible en: https://doi.org/10.1016/ S1473-3099(19)30312-3
Roden MM, Zaoutis TE, Buchanan WL, Knudsen TA, Sarkisova TA, Schaufele RL, et al. Epidemiology and outcome of zygomycosis: a review of 929 reported cases. Clin Infect Dis. 2005;41(5):634–653. Disponible en: https://doi.org/10.1086/432579
Skiada A, Lass-Floerl C, Klimko N, Ibrahim A, Roilides E, Petrikkos G. Challenges in the diagnosis and treatment of mucormycosis. Med Mycol. 2018;56(Suppl 1):93–101. Disponible en: https://doi. org/10.1093/mmy/myx101
Ramadorai A, Ravi P, Narayanan V. Rhinocerebral Mucormycosis: A Prospective Analysis of an Effective Treatment Protocol. Ann Maxillofac Surg. 2019;9(1):192-196. Disponible en: https://doi. org/10.4103/ams.ams_231_18
Jeong W, Keighley C, Wolfe R, Lee WL, Slavin MA, Kong DCM, et al. The epidemiology and clinical manifestations of mucormycosis: a systematic review and meta-analysis of case reports. Clin Microbiol Infect. 2019;25(1):26–34. Disponible en: https://doi.org/10.1016/j. cmi.2018.07.011
Lanternier F, Sun HY, Ribaud P, Singh N, Kontoyiannis DP, Lortholary O. Mucormycosis in organ and stem cell transplant recipients. Clin Infect Dis. 2012;54(11):1629–1636. Disponible en: https://doi.org/10.1093/ cid/cis195
Petrikkos G, Tsioutis C. Recent advances in the pathogenesis of mucormycoses. Clin Ther. 2018;40(6):894–902. Disponible en: https:// doi.org/10.1016/j.clinthera.2018.03.009
Spellberg B, Ibrahim AS. Recent advances in the treatment of mucormycosis. Curr Infect Dis Rep. 2010;12(6):423–429. Disponible en: https://doi.org/10.1007/s11908-010-0129-9
Hoenigl M, Seidel D, Carvalho A, Rudramurthy SM, Arastehfar A, Gangneux JP, et al. The emergence of COVID-19 associated mucormycosis: analysis of cases from 18 countries. Lancet Microbe. 2022;3(7):e543–e552. Disponible en: https://doi.org/10.1016/S26665247(21)00237-8
Munasinghe KVP, Silva FHDS. Rhinocerebral Mucormycosis with Extensive Cranial Nerve Palsies in a Diabetic Patient. Cureus. 2023;15(12):e50451. Disponible cureus.50451 en: https://doi.org/10.7759/
Caira M, Trecarichi EM, Mancinelli M, Leone G, Pagano L. Uncommon mold infections in hematological patients: epidemiology, diagnosis and treatment. Expert Rev Anti Infect Ther. 2011;9(7):881-92. Disponible en: https://doi.org/10.1586/eri.11.66
Millon L, Herbrecht R, Grenouillet F, Morio F, Alanio A, Letscher-Bru V et al. Early diagnosis and monitoring of mucormycosis by detection of circulating DNA in serum: retrospective analysis of 44 cases collected through the French Surveillance Network of Invasive Fungal Infections (RESSIF). Clin Microbiol Infect. 2016;22(9):e1-810.e8. Disponible en: https://doi.org/10.1016/j.cmi.2015.12.006
Smith C, Lee SC. Current treatments against mucormycosis and future directions. PLoS Pathog. 2022;18(10):e1010858. Disponible en: https://doi.org/10.1371/journal.ppat.1010858
Tawfik HA, Abdelhalim A, Elkafrawy MH. Computed tomography of the orbit - A review and an update. Saudi J Ophthalmol. 2012;26(4):40918. Disponible en: https://doi.org/10.1016/j.sjopt.2012.07.004
Ibrahim AS, Spellberg B, Walsh TJ, Kontoyiannis DP. Pathogenesis of mucormycosis. Clin Infect Dis. 2012;54(Suppl 1). Disponible en: https://doi.org/10.1093/cid/cir865
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Horizonte Médico (Lima)

This work is licensed under a Creative Commons Attribution 4.0 International License.
Horizonte Médico (Lima) (Horiz. Med.) journal’s research outputs are published free of charge and are freely available to download under the open access model, aimed at disseminating works and experiences developed in biomedical and public health areas, both nationally and internationally, and promoting research in the different fields of human medicine. All manuscripts accepted and published in the journal are distributed free of charge under the terms of a Creative Commons license – Attribution 4.0 International (CC BY 4.0).